Girls and Boys Suffer from HPV Vaccine Hair Loss
The teenage years are hard enough. Simply trying to deal with the normal stresses of school and a social calendar is enough trouble without trying to cover bald spots and find a way to look normal when all you feel is different. We post regularly about the obvious physical side effects of the Gardasil vaccine–Merck’s cervical cancer prevention vaccine that has been on the market since 2006–like Guillain Barre Syndrome, fainting, and weakness. But it isn’t often we talk about the side effects that affect the appearance and change body image and alter the self-esteem of many young ladies and women alike. Alopecia is an autoimmune disease that has been linked to Gardasil.
The FDA has officially acknowledged that alopecia areata, an autoimmune disease that causes hair loss, is a possible side effect of the HPV vaccine. In fact, according to the FDA’s September 2014 update on Gardasil: “As of December 31, 2013, VAERS had received 21 reports of alopecia areata following HPV vaccination, 18 in females and 3 in males. The median age of patients at the time of vaccination was 15 years (range: 11-19).”
This FDA acknowledgment is too little too late for the majority of teenagers who are suffering hair loss after their Gardasil vaccine. It is sometimes not until many years later that sufferers make the association between the vaccine and hair loss. This is a problem because the Vaccine Injury Compensation Program has a strict 3-year time limit to file a claim.
“My 12-year-old daughter was just diagnosed with alopecia areata. She received 2 doses of the Gardasil shot. Is this a coincidence? I will not be getting the 3rd shot. I believe Gardasil is the cause of this autoimmune disease [alopecia areata]. This shot is too new to be given to girls, more research is needed.” – Mother of Gardasil Victim
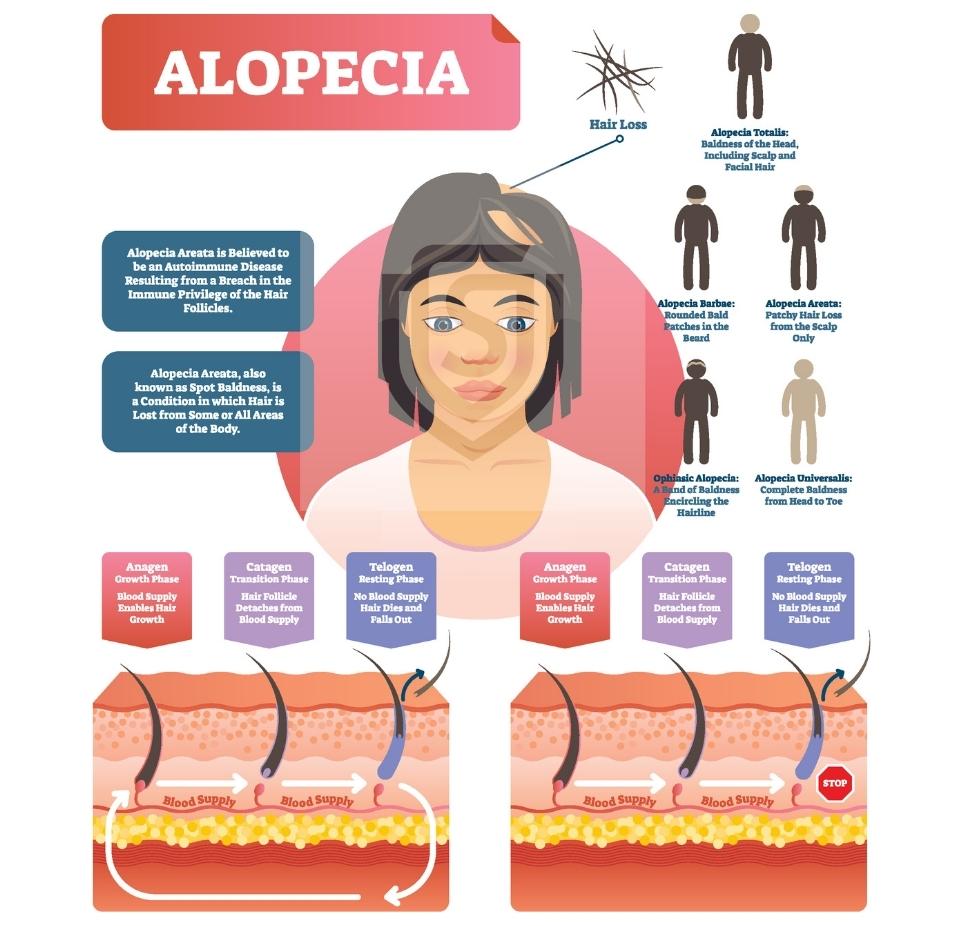
Most women who seek treatment for their dramatic hair loss after receiving Gardasil are often told one thing–Alopecia areata. Research surrounding this spotty form of hair loss shows that the condition is an autoimmune condition. As the body begins to attack certain tissues of the body (and in this case, perhaps the scalp and hair follicles) the hair is lost at a rapid rate, and more often on one side of the head than the other. Biopsies taken of skin show the presence of immune cells inside the hair follicles–a place where they would not normally be found. In some cases, though not as common, the alopecia can affect the entire body resulting in the loss of eyebrows, eyelashes, and everywhere else! Symptoms can begin as soon as a few weeks after vaccination.
What is alopecia areata?
Alopecia areata is an autoimmune disease that causes hair loss. The immune system attacks the hair follicles, causing them to become inflamed and preventing them from growing new hair. Alopecia areata can affect anyone of any age but is most common in teenagers and young adults. There is no cure.
What is Gardasil?
Gardasil is a human papillomavirus (HPV) vaccine that can help protect against certain types of cancer and other diseases caused by HPV. The original Gardasil HPV vaccine dose was three shots separated by a few months.
What are the known risks associated with Gardasil?
The most common adverse effects reported with Gardasil include pain, swelling, itching, redness, bruising, headache, and fever. Some people who receive Gardasil may also experience nausea, dizziness, fainting, and diarrhea. As with any vaccine, there is a risk of serious side effects. These may include allergic reactions, blood clots, and paralysis.
Does Gardasil cause alopecia?
Alopecia areata, an autoimmune disease that causes hair loss, is a possible side effect of the HPV vaccine. In fact, according to the FDA’s September 2014 update on Gardasil-related adverse events, there were at least 21 reports of alopecia following an HPV vaccine dose. While this may not sound like a lot, these events are rare.
Sadaka Law has been successful in obtaining compensation for young people suffering from Gardasil-related alopecia.
What are the types of alopecia?
There are several types of alopecia, each with different causes and effects. Here are some of the most common types:
Alopecia areata – This is a form of hair loss that usually affects the scalp, but can also affect other parts of the body. It’s thought to be an autoimmune condition, where the body’s immune system attacks the hair follicles.
Alopecia totalis – This is a rare form of alopecia that causes complete baldness of the scalp.
Alopecia universalis – This is the most extreme form of alopecia, causing complete baldness of the scalp and body. It’s very rare, affecting less than 1% of people with alopecia.
Androgenic alopecia – This is the most common type of hair loss, affecting both men and women as they age. It’s also known as “male pattern baldness” or “female pattern baldness”.
Scarring alopecia – This is a rare form of hair loss that’s caused by damage to the hair follicles. It can be caused by certain autoimmune conditions, infections, or even physical trauma. Scarring alopecia is usually permanent.
Telogen effluvium – This is a type of hair loss that can be caused by physical or psychological stress, pregnancy, childbirth, crash diets, iron deficiency, thyroid problems, and certain medications. It usually affects the whole head and can lead to thinning or shedding of the hair.
Traction alopecia – This is a type of hair loss that’s caused by tight hairstyles that pull on the hair (such as cornrows or ponytails). It’s usually reversible if you stop wearing the tight hairstyle.
What are the treatments for alopecia?
There is no cure for alopecia, but there are treatments that can help hair regrow more quickly. The most common treatment for alopecia areata is corticosteroid injections, which can help hair regrow in as little as two weeks. Other common treatments include topical corticosteroids, minoxidil ( Rogaine ), and Anthralin cream. In severe cases, doctors may recommend oral corticosteroids or immunosuppressive drugs.
What is erythema multiforme?
Erythema multiforme (EM) is a type of skin reaction that is often triggered by infections or medications. It results in red, raised bumps or welts on the skin that can be itchy or painful. In some cases, EM can also cause blisters or ulcers. While EM can occur at any age, it is most common in young adults. EM is not contagious and usually goes away on its own within two to four weeks. However, severe cases may require treatment with steroids or other medications. It can occur after Gardasil and is a separate condition from alopecia.